What are Medical Claims?
After a patient has visited a doctor, hospital, or other health care provider a bill is generated and then submitted to the health insurance carrier as a medical claim. The medical claim is then processed by the insurance carrier for payment.
Including the diagnosis and services rendered accurately is essential during the medical claims process. An error in the medical claim can cause unnecessary back and forth between the patient, insurer, and medical practice and can even risk the claim being denied entirely. Due to this, it is important that the medical claim be checked for errors before it is submitted.
How is a Claim Created?
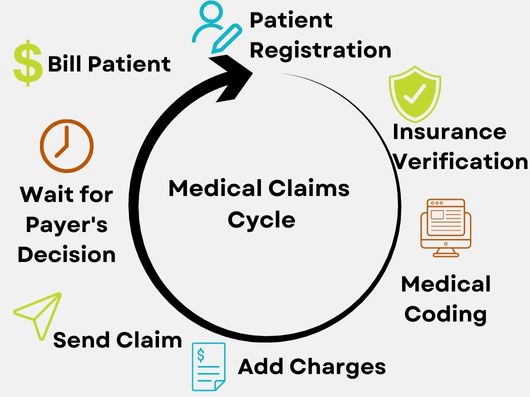
The claim creation process is long and starts before the patient arrives at their appointment. When creating a claim the following steps must be followed:
- 1. Patient Registration: Prior to the appointment, the patient's health information and personal details are collected. Many practices use management software that makes this easier.
- 2. Verification of Insurance Benefits: Once the insurance information is gathered it is typically verified to ensure that the visit is covered under the patient's insurance policy. This also helps determine what the patient's copay is and if the patient needs pre-approval. Copays are important for medical providers as it adds to their cash flow while they wait for payer reimbursement.
- 3. Medical Coding: After the care services have been administered the visit notes are sent to the medical coder, who transcribes the documentation into a standardized medical code. These codes are used to describe what medical procedures, diagnoses, prescriptions, and supplies were administered during the visit.
- 4. Add Charges: After the medical coding is completed, all the charges need to be added to the claim before sending it to the payer.
- 5. Send Claim: Claims are transferred to the payer. Usually, the claims will first be sent to the clearinghouse, where they are reviewed and reformatted before sending the finalized version to the payer.
- 6. Wait for Payer’s Decision: Often referred to as adjudication, the payer determines whether to accept, deny, or reject the claim. If the claim is accepted the payer then determines the amount of reimbursement. Reimbursement isn’t always 100%, the payer can pay only the part that is owed and the patient will be responsible for the remaining balance.
Sometimes claims are rejected or denied. Rejections can be frustrating, but are often easily resolved by resubmitting the claim with all errors fixed. Denials are harder to address. They can be denied for a variety of reasons, including lack of pre-authorization or insufficient patient coverage. Regardless of the reason, the patient can file an appeal to their insurer. This process can be lengthy, so payment will be delayed. - 7. Patient Registration: All remaining balances are then billed to the patient.
How is a Claim Filed?
Occasionally, the patient will have to file the claim themselves, often times this happens when they see a doctor that is out of their network. In this case, the patient should follow these steps:
- 1. Log in to your insurance website and find the correct form that aligns with your benefit plan.
- 2. If possible, fill the form out online. If unable to complete the form online, it can be done by hand, but ensure that handwriting is readable and the form is filled out correctly.
- 3. Include all details from your visit including the date of service and all the medical codes that were provided by the physician's office.
- 4. Make sure to check claim filing deadlines and file before the due date.
- 5. Double-check that the service you were provided is covered by your insurance plan before submitting the claim, otherwise, it will come back as denied.
- 6. If applicable, include all signed pre-approval forms with your claim submission.
- https://www.definitivehc.com/blog/medical-claims-101-what-you-need-to-know
- https://www.businessnewsdaily.com/16237-medical-claims-how-to.html
- https://sdata.us/2020/12/15/the-medical-claims-process-a-simplified-guide/
Learn More
Are you interested in learning more about the medical billing and claims process? U.S. Career Institute has a variety of information available in our Healthcare Blog. If you are interested in pursuing a career as a medical claims and billing specialist check out our certificate program.
Sources:
